Atrial Septal Defect (ASD) Surgery

Atrial Septal Defect
An atrial septal defect (ASD) is a congenital heart defect that involves a hole in the atrial septum. This is the muscular wall that separates the two upper chambers (atria) of the heart. Small ASDs usually don’t need treatment. Larger ones may require percutaneous (nonsurgical) repair or surgery to lower the risk of serious complications.
Overview
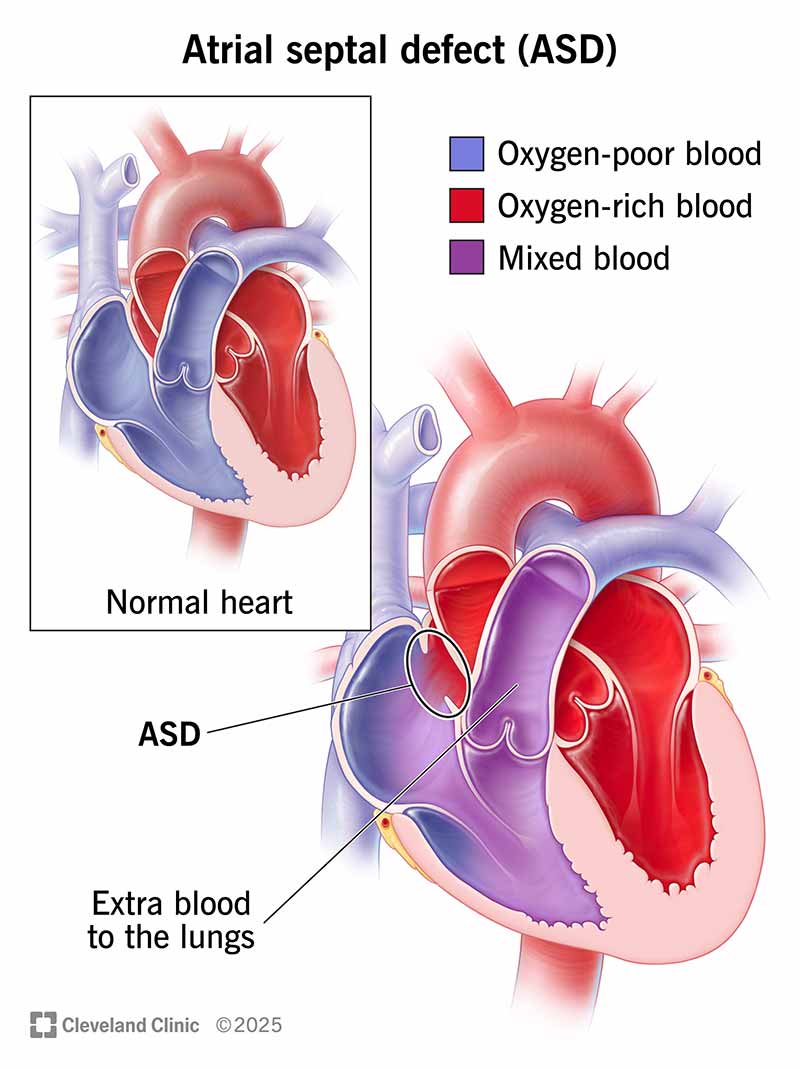 Normally, oxygen-rich blood flows from your left atrium to your left ventricle and then out to your body. An ASD causes some of that blood to travel into your right atrium, where it mixes with oxygen-poor blood and flows back to your lungs.
Normally, oxygen-rich blood flows from your left atrium to your left ventricle and then out to your body. An ASD causes some of that blood to travel into your right atrium, where it mixes with oxygen-poor blood and flows back to your lungs.What is an atrial septal defect?
An atrial septal defect (ASD) is a hole in the atrial septum, which is the wall that separates your heart’s two upper chambers (atria). An ASD is a congenital heart defect (something you’re born with) that happens when the septum doesn’t form properly. It’s also called a “hole in the heart.”
An ASD allows an abnormal shunt, meaning an abnormal passageway for blood that shouldn’t be happening. Normally, oxygen-rich blood flows from your left upper chamber (atrium) down to your left lower chamber (ventricle), and then out to supply oxygen to your body. An ASD causes some blood from your left atrium to flow in the wrong direction, into your right atrium. Your right atrium contains oxygen-poor blood that needs to cycle through your lungs. So, your right atrium now has extra blood that ultimately goes to the lungs.
This wrong-way leak might be minor and not cause any problems. In those cases, the ASD can be left alone without treatment. Other times, it can lead to problems with your heart or lungs. The bigger the ASD, the more likely it is to cause symptoms and need treatment.
What are the different types of atrial septal defects?
There are four main types of atrial septal defects. They’re defined by their location in the atrial septum.
Secundum ASDs are in the middle of your atrial septum. This is the most common type of ASD, (80% of all ASDs).
Primum ASDs are in the lower part of your atrial septum. Babies with primum ASDs may also have other heart defects. These include endocardial cushion defect, atrioventricular septal defect, tricuspid valve defects and mitral valve defects. Primum ASDs are commonly linked with Down syndrome.
Sinus venosus ASDs are in the upper or lower back part of your atrial septum. This type is linked with defects in the right pulmonary vein or large veins in the heart called superior or inferior vena cava.
Unroofed coronary sinus is the rarest type of ASD (less than 1% of all ASDs). It involves a missing or incomplete wall between your coronary sinus (a group of veins connected to your heart) and your left atrium. It's more often linked with another complex congenital heart disease.
How common are atrial septal defects?
An atrial septal defect is one of the most common types of congenital heart defects in children. It occurs in approximately 1 to 2 out of 1,000 live births. About 1 in 1,859 babies are born with an atrial septal defect in the U.S. This adds up to about 2,118 babies born with ASD each year.
What conditions are associated with atrial septal defects?
Some babies born with an atrial septal defect also have other heart defects or genetic disorders. Some associated heart defects include:
Mitral valve disease.
Pulmonary stenosis.
Associated genetic disorders include:
Holt-Oram syndrome.
Thrombocytopenia-absent radii (TAR) syndrome.
What is the difference between an atrial septal defect and a patent foramen ovale?
An atrial septal defect (ASD) and a patent foramen ovale (PFO) are both openings in the atrial septum. But ASD is a congenital heart defect, meaning it’s a problem that occurred while a fetus was still in the uterus. Septal tissue should’ve formed in that part of the atrial septum, but didn’t. So a baby is born with a hole in their heart.
A patent foramen ovale isn’t a congenital heart defect. Tissue isn’t missing from the atrial septum. Instead, a PFO happens when a normal flap-like opening in a baby’s heart (foramen ovale) doesn’t seal shut after birth. The foramen ovale is normal, and we all have one when we’re born. This is a normal pathway to allow oxygen-rich blood from the placenta to circulate to the fetus’ brain while in the uterus.
When we’re born, we no longer need the foramen ovale since our lungs start working. So it usually closes on its own soon after birth and completely seals off in a couple of days or weeks after. When it doesn’t close on its own, it’s called a patent foramen ovale. “Patent” means open or failing to close.
A PFO is usually smaller than an ASD. That’s why it doesn’t usually cause any problems or symptoms. The risk of symptoms and problems goes up when an opening in the septum is bigger.
PFOs are much more common than ASDs. Estimates show that about 1 in 4 adults have a PFO. Most people never know they have this small opening in their hearts. It’s usually harmless, but people who have a PFO along with heart problems such as atrial fibrillation may face a higher risk of a stroke.
How does an atrial septal defect affect a person’s body?
A small ASD doesn’t affect your body much. But larger ASDs can strain the right side of your heart. That’s because the right side of your heart now has extra blood it must pump out to your lungs. Plus, this extra blood flow can slowly damage the blood vessels in your lungs.
Problems with large ASD include:
Right heart enlargement, which can lead to heart failure if left uncorrected for a very long period of time.
Abnormal heart rhythm (arrhythmia), including atrial fibrillation or atrial flutter. At least half of adults over age 40 with an ASD have an arrhythmia.
Pulmonary hypertension. This is high blood pressure in the arteries that supply blood to your lungs.
Eisenmenger syndrome. This condition can happen in people who have an ASD along with severe pulmonary hypertension.
Symptoms and Causes
What are the symptoms of an atrial septal defect?
Even though an atrial septal defect is present at birth, many people don’t have symptoms until far into adulthood. Small ASDs (less than 5 millimeters) may not cause symptoms because they don’t strain the heart or lungs.
Symptoms of an ASD in children
Most children have no signs or symptoms. The most common (and often the only) sign will be a heart murmur. Their healthcare provider will notice it when listening to their heart with a stethoscope.
When children do have other symptoms, they include:
Being underweight.
Growth delays.
Recurrent respiratory infections.
Although extremely rare, children with larger ASDs may have symptoms that include:
Easily becoming fatigued when exercising.
Trouble breathing.
Tell your child’s provider about any symptoms you notice. Their provider may want to run some tests to check your child’s heart structure and function.
Symptoms of an ASD in adults
Adults with ASD may feel symptoms by age 40. Symptoms depend on how much the ASD has strained the heart and lungs. They include:
Shortness of breath with exercise.
Fast heartbeat (tachycardia).
Swelling in the arms and legs.
Blue skin color (cyanosis).
If you have any of these symptoms, call your healthcare provider right away. These symptoms could mean you have an untreated ASD. Or, they could mean you have another cardiovascular problem that needs treatment. If you have chest pain, you should call 911 or your local emergency number.
What causes atrial septal defects?
The exact cause of atrial septal defects isn’t fully known. However, congenital heart defects are often caused by genetic changes that happen before birth. Some genetic mutations associated with ASD affect the NKX2.5/CSX and TBX5 genes.
Some factors can raise a birthing parent’s risk of having a baby with congenital heart disease. These factors include:
Alcohol consumption.
Smoking and tobacco use.
Taking certain prescription medications.
Diagnosis and Tests
How are atrial septal defects diagnosed?
Atrial septal defects are diagnosed through a physical exam along with tests that check your heart’s structure and function.
Tests to diagnose atrial septal defects
Your provider will run one or more tests to diagnose you with an ASD and learn how it’s affecting your heart. These include:
Electrocardiography (ECG/EKG). An ECG shows your heart’s electrical activity. It can reveal if you have an arrhythmia or other problems related to your heart’s electrical system.
Chest X-ray. This test will show if your right atrium and right ventricle are enlarged. It’ll also show if the blood vessels in your lungs are affected.
Transthoracic echocardiography (TTE). This test shows how the left-to-right shunting of blood (caused by ASD) affects your heart. It can also show details related to pulmonary hypertension.
Transesophageal echocardiography (TEE). A TEE is an ultrasound taken through your esophagus. It shows the size, shape and location of an ASD. It can also check your heart valves. TEE is often used during ASD surgery and percutaneous repair.
Intracardiac echocardiography (ICE). This is an ultrasound taken inside your heart. A tiny camera (echo probe) is sent to your heart through a peripheral vein. This test shows the size and shape of the ASD and the direction of the blood flow across it. It’s often used during percutaneous (nonsurgical) repair of ASD.
In some cases, Cardiac CT scan or Heart MRI may be used. They’re most helpful for people with associated defects or less common forms of ASD.
Management and Treatment
What is the treatment for an atrial septal defect?
Atrial septal defects can be closed through surgery or percutaneous (nonsurgical) repair.
The type and timing of ASD treatment depends on many factors, including:
ASD type and size.
How the ASD is affecting your heart.
Other conditions you have, like pulmonary hypertension, valve disease or coronary artery disease.
Small ASDs usually don’t need repair. However, larger ASDs should be repaired even if they aren’t causing symptoms. This prevents serious complications down the road.
Once you have signs of heart or lung damage, repair is essential. Your provider will recommend treatment if:
The right side of your heart is bigger than normal.
There’s significant shunting (flow of blood through the ASD).
Your provider may prescribe medications to treat some symptoms of ASD. But there aren’t any medications that can close the hole.
If you have pulmonary hypertension, you may need to take medication before your repair procedure. This medication treats pulmonary hypertension and makes the procedure safer for you.
Percutaneous (nonsurgical) repair of ASDs
This type of repair uses a device (called a septal occluder) to close the hole in your atrial septum. The device is put in place using a long, thin tube called a catheter. The occluder is attached to the catheter, which is guided to your heart through a vein in your groin. When the occluder is released from the catheter, it opens up and seals the hole. Over time, tissue grows over the occluder, and it becomes part of your heart.
Percutaneous repair can close most secundum ASDs and some sinus venosus ASDs. So, this is the method used most often.
Before the repair, you’ll have a cardiac catheterization to check the size and location of the ASD and measure pressures in your heart.
After the repair, you’ll take blood-thinning medication (anticoagulant or antiplatelet) to keep blood clots from forming on the device (a possible but rare complication). Your provider will talk with you about the right type of medication for you and how long you need to take it.
Surgical repair of ASDs
Surgery is needed for primary ASDs, coronary sinus defects and most sinus venosus ASDs. These are rare defects that require treatment by a cardiac surgeon with expertise in congenital heart disease. Robotic-assisted surgery or minimally invasive surgery may be options for some people.
A surgical repair usually involves using a tissue patch to close the ASD. The tissue often comes from your own pericardium (the membrane around your heart). Some secundum ASDs can be surgically closed with just sutures and no patch.
Prevention
Can atrial septal defects be prevented?
There’s no specific way to prevent atrial septal defects. They develop when a fetus is still in the uterus. But prenatal care may impact a fetus'schances of having congenital heart disease. If you’re pregnant or planning a pregnancy, it’s important to:
Quit smoking and using tobacco products.
Avoid drinking alcohol.
Avoid secondhand smoke.
Avoid using recreational drugs, especially cocaine.
Talk with your provider about any prescription medications you’re taking and how those might affect your pregnancy.
Genetic testing may be helpful if you or other biological family members have congenital heart disease.
Outlook / Prognosis
What is the life expectancy of someone with an atrial septal defect?
People with an ASD may have a lower life expectancy than those without an ASD. Life expectancy depends on many factors, including the size of the ASD and whether you have ASD repair. The timing of repair also matters. Research shows that people who have ASD repair earlier in life have a better outlook. This is likely because early repair catches the problem early before it can cause serious damage to your heart or lungs.
People who need ASD repair but don’t have it by age 40 face the greatest danger. Their risk of death goes up by 6% with each passing year.
Living With
When should I see my healthcare provider?
If you’ve been diagnosed with an ASD, it’s important to keep all your medical appointments and follow your provider’s guidance. Heart defects like ASD often call for “watchful waiting.” This means your provider keeps an eye on the situation to see when you need treatment. Your provider will tell you how often you need to come in for appointments.
If you’ve had ASD repair, you should follow your provider’s guidance for follow-ups. You’ll likely go back for follow-ups:
One month after your procedure.
Three months after your procedure.
Six months after your procedure.
Twelve months after your procedure.
And then once a year after that.
If your child has an ASD, their provider will let you know the next steps and when intervention might be needed. In general, small ASDs are treated with “watchful waiting.” Larger ASDs usually require procedures at a younger age to prevent problems later on. Talk with your child’s provider to learn more about the best treatment plan for them.
How should I take care of myself?
People with an atrial septal defect should follow their provider’s guidelines for at-home care and medical follow-ups. After ASD repair, you’ll likely have activity restrictions for a while as you recover. You’ll also need to take medications such as:
Blood thinners (anticoagulants or anti-platelets). You’ll need these for six to 12 months following repair. But if you had a stroke, you may need them long-term.
Antibiotics. These are needed before certain medical procedures. You usually need to take this precaution for at least six months following your repair. Antibiotics prevent an infection of your heart’s lining (endocarditis).
Other medications. If you have another heart condition, you may need to take other medications as prescribed by your healthcare provider.
After you’ve recovered from ASD repair, it’s still important to do whatever you can to take care of your cardiovascular system. Work with your provider to learn how you can reduce your risk of future heart and vascular problems. Your provider may offer suggestions including:
Following a heart-healthy diet.
Adding more physical activity and planned exercise to your days.
Quitting smoking or reducing alcohol consumption.
Finding ways to manage stress in your daily life.
Call your provider any time you have questions or concerns. Thanks to advances in diagnosis and treatment, people with ASDs have a good outlook for a fruitful and enjoyable life.
